Rudolf Virchow : Medicine and Surgery – Beacon Lights of History, Volume XIV : The New Era by John Lord
John Lord – Beacon Lights of History, Volume XIV : The New Era
Richard Wagner : Modern Music
John Ruskin : Modern Art
Herbert Spencer : The Evolutionary Philosophy
Charles Darwin : His Place in Modern Science
John Ericsson : Navies of War and Commerce
Li Hung Chang : The Far East
David Livingstone : African Development
Sir Austen Henry Layard : Modern Archaeology
Michael Faraday : Electricity and Magnetism
Rudolf Virchow : Medicine and Surgery
John Lord – Beacon Lights of History, Volume XIV : The New Era
by
John Lord
Topics Covered
Jenner demonstrates efficacy of vaccination against smallpox.
Debt to the physicists, chemists, and botanists of the new era.
Appendicitis (peritonitis), its present frequency.
Experimental methods of study in physiology.
Hahnemann, founder of homoeopathy, and physical diagnosis of the sick.
The clinical thermometer and other instruments of precision.
Animal parasites the direct cause of many diseases.
Bacteria and the germ theory of disease.
Pasteur, viruses, and aseptic surgery.
Consumption and its germ; the corpuscles and their resistance to bacterial invasion.
Antitoxines as a cure in diphtheria.
Their use in surgery; asepticism and Lord Lister.
Listerism and midwifery.
American aid in the treatment of fractures.
Use of artificial serum in disease treatment.
Koch’s tuberculin and its use in consumption.
Chemistry as a handmaid of medicine.
Brown-Séquard and “internal secretions”.
Febrile ailment and cold-water applications.
Surgical anaesthetics; Long, Morton, and Simpson.
Ovariotomy operations by McDowell and Bell.
Professional nursing.
Virchow and the literature of medicine, anatomy, and physiology; his death;
his “Archiv,” “Cellular-Pathology,” etc.
Rudolf Virchow : Medicine and Surgery
By Frank P. Foster, M.D.
1821-1902.
Stagnation was the state of medicine when the Nineteenth Century opened. It was only three years before that Jenner had announced and demonstrated the protective efficacy of vaccination against small-pox. His teaching, in spite of the vehement cavillings of the “antis” of his day, gained credence readily, and vaccination speedily became recognized and was constantly resorted to, but hardly any attempt at perfecting the practice was made until after more than fifty years had elapsed. His discovery–or, rather, his proof of the truth of a rustic tradition–fell like a pebble into the doldrums; the ripple soon subsided, and nobody was encouraged to start another. At the present time such an announcement would be promptly followed by investigations leading up to such doctrines as that of the attenuation of viruses and that of antitoxines. But the times were not ripe for anything of that sort; medicine reposed on tradition, or at best gave itself only to such plausibilities in the way of innovation as were cleverly advocated. Physicians strove not to advance the healing art; as individuals, they were content to rely on their manners, their tact, and their assumption of wisdom. In short, the body medical was in a state of suspended animation, possessed of a mere vegetative existence.
The Humoral pathology, or that doctrine of the nature of disease which ascribed all ailments to excess, deficiency, or ill “concoction” of some one of the four humors (yellow and black bile, blood, and phlegm), had not yet lost its hold on men’s convictions, or at least not further than to make them look upon exposure to cold and errors of diet as amply explanatory of all diseases not plainly infectious. The medical writers who were most revered were those who busied themselves with nosology; that is to say, the naming and classifying of diseases. Wonderful were the onomatological feats performed by some of these men, and most diverse and grotesque were the data on which they founded their classifications. To label a disease was high art; to cure it was something that Providence might or might not allow. In the treatment of “sthenic” acute diseases (meaning those accompanied by excitement and high fever), blood-letting, mercury given to the point of salivation, antimony, and opium, together with starvation (all included under the euphemism of “lowering measures”), were the means universally resorted to and reputed “sheet anchors.” Some advance had been made from the times when disease had been looked upon as an entity to be exorcised, but it was still so far regarded as a material thing that it was to be starved out.
But the century was not out of its second decade when signs of an awakening from this lethargy began to show themselves. The first steps, naturally, were along preparatory lines, and for those we are largely indebted to the physicists, the chemists, and the botanists. Gross anatomy became better known, owing for the most part to more enlightened legislation on the subject of the dissection of the human body; minute anatomy (histology) sprang into existence as the result of improvements of the compound microscope. Physiology took on something of the experimental; and medication was rendered far less gross and repulsive by the isolation of the active principles of medicinal plants. But it was long after all this that the telling strides were taken. Up to within the memory of many men who are now living, “peritonitis” tortured its victims to death, said “peritonitis” being often interpreted as a manifestation of rheumatism, for example, and no well-directed interposition was attempted against it, whereas we now know perfectly well that the vast majority of cases of peritonitis are due to local septic poisoning and for the most part quite readily remediable by the removal (with a minimum of danger) of the organ from which such poisoning arises–almost always the vermiform appendix. “Appendicitis,” of which we hear so much nowadays, is no new disease; it is simply the “peritonitis” that killed so many people in former times. But while no well-informed person would now maintain that this disease was a new one, there are many, and those, too, among the best instructed, who find it difficult to avoid the conclusion that, if not new, it must at least be of far more frequent occurrence than formerly. It must be borne in mind, however, that in the great majority of instances in past years it ended spontaneously in recovery and was forgotten.
Two features of the progress in medicine in the Nineteenth Century, negative as they may seem to have been, were undoubtedly potent in the promotion of advance. They were the recognition of the fact that many dangerous diseases are self-limited, and the experiment of the so-called “expectant treatment.” The result of the first of them was to teach men to desist from futile attempts to cure the self-limited diseases, in the sense of cutting them short in their course, and the “expectant treatment” followed as a natural consequence. It was a method of managing disease rather than attempting to cure it. There was no interference save to promote the patient’s comfort, to nourish him as thoroughly as might be without unduly taxing his powers, and to meet complications as they arose. It was stooping to conquer, perhaps, but it was a policy that conduced greatly to the well-being of the sick, improved their chances of recovery, and enabled physicians to study disease more accurately by reason of its course not being rendered irregular by meddlesome medication. It has never been dropped, and it never will be, save as such directly curative agents as the antitoxines are made available.
In the early part of the century, except for gross anatomy and operative surgery, medicine was taught almost wholly, so far as the schools were concerned, by means of didactic lectures. The “drawing” capacity of a professor was proportionate rather to his rhetorical powers and to the persuasiveness with which he inculcated the views peculiar to himself than to the amount of real information that he conveyed to the students. Although the apprentice system–for that was what the practice of students’ attaching themselves to individual practitioners, whom they called their preceptors, virtually amounted to–in many instances made up more or less completely for the lack of systematic clinical teaching, yet in the great majority of cases it amounted to little more than the preceptor’s allowing the student the use of his library and occasionally examining into the latter’s diligence and intelligence, in return for which he, the preceptor, required an annual fee and exacted from the student such minor services as his proficiency enabled him to render. It is true the students “walked” the hospitals, drinking in some great man’s utterances, but they did it in droves, not a moiety of them being able to get a good look at a patient, unless it was such a passing glance as might tell them that the patient was jaundiced. By clinical teaching we understand teaching, not in glittering generalities, but in the concrete, either at the bedside, as the word clinical originally implied, or at least with the patient actually present to illustrate in his person the professor’s descriptions and the success or failure of the treatment employed. The clinic is now firmly established, and has been for years, but it was long before this grand result was attained.
Experimental methods of study gradually came into vogue, particularly in the domain of physiology. In this sphere Dr. William Beaumont, of the United States Army, was a pioneer. His historic experiments on Alexis St. Martin, a soldier who had been wounded in the stomach and recovered with a permanent opening into that organ, will ever rank among the most important of the early experimental studies of digestion. It was not long before Claude Bernard extended similar inquiries to the other functions of the body, notably those of the nervous system; and since his time there has been a long array of brilliant investigators of physiology and of other branches of science tributary to medicine. Experiments on living animals were almost the only means of carrying on these researches. In the early days the animals employed were doubtless put to a great deal of pain–perhaps in many instances to unnecessary suffering–and an altogether laudable feeling of humanity has led good people to band themselves together for the purpose of putting a stop to vivisection, or at least of greatly restricting the practice and of freeing it from all avoidable infliction of pain. These praiseworthy efforts have in some instances been carried so far, unfortunately, as to seriously hamper scientific investigation–investigation which has for its object the alleviation of human suffering and the saving of human life. We may earnestly deprecate and strive to prevent wanton reiteration of painful experiments for purposes of demonstrating anew that which is unquestioned, and we may resort to all possible means to render necessary experiments free from actual pain (from the anguish of trepidation we can seldom relieve the poor animals), but let us not block the wheels of scientific progress.
At the dawn of the Nineteenth Century, to examine a sick person’s pulse, to inspect his tongue, to observe his breathing, to interrogate his skin by our sense of touch, and to try to make his statements and those of his friends fit in with some tenable theory of the nature of his ailment, were about all we could do. Possibly it was because he realized to an uncommon degree the tremendous impediment of this narrow limitation that Samuel Hahnemann, the founder of Homoeopathy, cut the Gordian knot in sheer rebelliousness, and proclaimed, as he virtually did, that a diagnosis was not necessary to the successful treatment of disease, but that one only needed to know empirically how to subdue symptoms, meaning mainly, if not solely, what we term “subjective” symptoms–those of which the patient complains, as opposed to those that we ourselves discover. But the physical examination of the sick, before extremely meagre in its sphere and restricted in its possibilities, was destined to expand before many years into the minute and positive physical diagnosis of the present day.
In the year 1816 a French physician, Réné Théophile Hyacinthe Laennec, achieved undying fame by publishing to the world an account of his labors in the application of mediate auscultation and of percussion to the diagnosis of the diseases of the chest. It is true that no less a personage than the “Father of Medicine,” Hippocrates, is reputed to have practised succussion as a means of diagnosis; that is, the shaking of a patient, as one would shake a cask, to ascertain by the occurrence or non-occurrence of a splashing sound if the person’s pleural cavity was distended partly with water and partly with air. It is probable that Hippocrates and many others after him carried the physical examination of the chest still further, for it is difficult to imagine, for example, that so simple a device as that of thumping a partition to make out the situation of a joist by the sound evoked should not early have been applied to the human chest. But, be this as it may, to Laennec belongs the great credit of having laid a substantial foundation for the physical diagnosis of the present time, and, more than for laying a foundation, for constructing a fairly complete edifice. He who should now undertake to practise general medicine without having first made himself proficient in the detection and interpretation of the sounds elicited by auscultation and percussion in diseases of the heart and lungs would foredoom himself to failure.
It was not until many years later, early in the second half of the century, that the clinical thermometer came into general use, but it soon showed most strikingly the superiority of the “instrument of precision” to the unaided senses of man. Who would think now of trying to estimate the height of a fever by laying his hand on the patient’s skin, or who, even among the laity, would be satisfied with such a procedure? “Doubtless,” said the present writer in a former publication (“New York Medical Journal,” Dec. 29, 1900), “the use of the thermometer has occasionally given rise to needless alarm, but almost invariably it may be interpreted with great certainty. Often it dispels unnecessary anxiety as in a twinkling by its negative indication, and surely it is to be credited with being distinctly diagnostic in those diseases of which it has itself established the ‘curve.'” By the thermometric “curve” of a disease is understood the general visual impression made by the graphic chart of a temperature record–the course of a zigzag line connecting the points indicated by the various individual observations.
Numerous other instruments of precision are now in constant use, among the most wonderful of which perhaps is the ophthalmoscope, whereby we are enabled to subject the retina and the intervening media of the eye to minute visual examination. There is not an organ of the body that is not now interrogated daily in the way of physical diagnosis, and we even examine separately the secretion of each of the two kidneys. In addition, there are multitudinous specific signs of which we were not long ago in complete ignorance. To cite only one of these, there is Widal’s agglutination test, by which the bacteriologist can usually make a diagnosis of typhoid fever far in advance of the time at which it could otherwise be distinguished. The use of the Röntgen rays in diagnosis was one of the crowning achievements of the century, and now we seem about to enter upon a course of their successful employment in the treatment of disease–even some forms of cancer–as well as in its detection.
Beyond the vermin that infest the skin and the hair, tapeworm, and a few other intestinal worms, little if anything was known of morbific parasites before the Nineteenth Century; but the labors of Van Beneden, Küchenmeister, Cobbold, Manson, Laveran, and others have now established the causal relationship between great numbers of animal parasites–gross and microscopic–and certain definite morbid states. This has led to a great increase in our knowledge of the connection between the parasites of the lower animals and grave disease in human beings, and on this knowledge rest many of the precautions that we are now able to take against the spread of such disease. From the consideration of animal parasites as the direct causes of disease, we naturally come to the contemplation of the subject of insects as the carriers of disease. The later years of the century have witnessed the demonstration of the fly’s agency in the transmission of malignant pustule and typhoid fever, and that of certain mosquitoes in the conveyance of yellow fever and malarial disease. We now know that bad air (the original meaning of the word malaria) has nothing to do with fever and ague, and that swamps are not unwholesome if they are free from infected mosquitoes. The mosquito does not originate the malarial infection; it simply serves as the temporary host of the micro-organism (Plasmodium malarioe) which is the cause of the disease, having obtained its transient “guest” from some human being. Consequently, marshy districts that are full of mosquitoes are not malarious unless the mosquitoes are of the kinds capable of lodging the plasmodium, and unless there is or has recently been present in the neighborhood some person affected with malarial disease. Moreover, the most virulently malarious region is a safe place of residence for human beings, provided they protect themselves absolutely against the bite of the mosquito. This has been strikingly demonstrated in the case of the Roman Campagna.
From the disease-producing animal parasites we come now to those that are believed to be of vegetable nature. Under the general name of bacteria, there are multitudes of micro-organisms having pathogenic powers, each giving rise to some definite specific disease, and certain associations of different bacteria causing particular morbid conditions. Generations ago physicians had a glimmering of what we now term the germ theory of disease, as was shown by their use of such expressions as materies morbi and morbid poisons. Even the definite relationship of special microscopic organisms to individual diseases was foreshadowed by Salisbury nearly fifty years ago. But it was not until years after those conceptions, and in no wise descended from or led up to by them, that an intelligible and satisfactory germ theory of disease was formulated.
It is to Pasteur, the immortal chemist, that we owe this theory, as well as that of the attenuation of viruses–both of more than theoretical import, since they have given us aseptic surgery, the power of frequently preventing hydrophobia, the antitoxine treatment of diphtheria, and the ability to stay the hand of Death in the form of many a stalking pestilence. Every infectious disease is now held to be due to its own particular micro-organism, and many diseases that were not until recently thought to be infectious are now classed as such because they have been proved to be caused by living germs. Conspicuous among these diseases is pulmonary consumption. In the case of almost every one of these diseases we have discovered the specific germ and are able to demonstrate its presence, either by its microscopical appearance, by its behavior on contact with certain stains, or by the forms that cultures of it assume. The micro-organism of small-pox and that of cancer (the existence of which is assumed) have not yet been isolated. Some of these germs, like that of tetanus (lockjaw), gain entrance to the system only through a wound; others, like those of typhoid fever and cholera, are swallowed; others, like that of pneumonia, are inhaled; still others, like that of tuberculous disease, are either swallowed or inhaled. Some are believed to be transmissible to the unborn child; and a few are ordinarily harmless parasites, becoming pathogenic only when they accidentally gain access to other parts of the system than those which constitute their natural habitat.
These microscopic organisms do not by their mere presence set up disease, unless indeed they are in such overwhelming numbers as to block the capillary blood vessels mechanically. Some of them are carried broadcast in the blood current, while others remain at the point of entrance; in either case they elaborate certain products, termed toxines, which act, either locally or through the circulation, to cause the disease. These toxines eventually kill the micro-organisms that produced them, quite as an animal may be smothered in its own exhalations; or at least they would do so if the “host” survived long enough for the completion of the process. Meantime, they have either killed the “host” or been defeated by certain very interesting natural processes. But before either of these occurrences has had time to take place, fortunately, in the great majority of instances, save those of exposure to the most deadly of infections, the vital power of the invaded individual has coped successfully with the invaders at the very point of attack–has repulsed the attacking party without appreciable impairment of its own force–and no illness results. For example, practically all of us inhale the germ of consumption repeatedly, but most of us suffer no harm from it simply because the fluids which bathe the surface on which the germ effects a lodgment are endowed with properties which either kill the germ or rob it of its power for harm; but these properties suffice only when the general health is unimpaired.
In case the attack is not successfully repelled at the outset, what happens? There begins a struggle between the invaders and what may be called the reserves of the organism, consisting of the white blood corpuscles, which undergo a great augmentation in number. These corpuscles are endowed with the faculty of amoeboid movement; that is to say, they may shoot out projections from their substance, and even convert themselves for the time being into traps, seizing upon the pathogenic bacteria, incarcerating them within their own mass, and carrying them away to be thrust out of the system by organs whose function it is to eliminate extraneous matter. These corpuscles are, indeed, said figuratively to eat the malign micro-organisms, whence they have been termed phagocytes (from [Greek: phagein], to eat, and [Greek: kutos], a cell); also because they carry away refuse and noxious material, they have been called “the scavengers of the system.” By means of their amoeboid movement they are enabled to worm themselves through inconceivably minute apertures in the blood vessels, and attack and devour peccant matter wherever it may have effected a lodgment. These white corpuscles are also known as leucocytes, and their increase in number when they are called upon to resist bacterial invasion is spoken of as hyperleucocytosis. The discovery of their protective function is to be credited to Metchnikoff, a Russian physician now teaching in Paris. When they migrate from the blood vessels in great numbers they finally, after having fulfilled their office as phagocytes, degenerate into the corpuscular elements of pus, which is the creamy liquid contained in an abscess. Their migratory power was discovered by Cohnheim.
But as a general thing the phagocytes do not succeed in making away with all the pathogenic germs, or even with enough of them to prevent the illness which they tend to produce. The further combat is between the poisonous products, termed toxines, engendered by the bacteria and certain antidotal substances, called antitoxines, newly created in the watery portion of the blood by some wonderful provision of Nature that is not yet well understood. Each infective disease has its special toxine, and for the destruction of each the blood prepares its particular antitoxine; possibly, however, some of the antitoxines may be efficacious against more than one kind of toxine, for there are physicians who are convinced that vaccination is a temporary preventive of whooping-cough. But the elaboration of an antitoxine takes time, and the result in any given case, whether in recovery or in death, seems to be settled by the ability or inability of the vital powers of the individual to hold out until they are relieved by the evolution of the necessary amount of antitoxine.
In the long run, provided the sick person survives, more antitoxine is generated than is required to save life. The excess remains in the system for a greater or lesser length of time, and this fact explains the individual’s subsequent immunity to the disease from which he has recovered; any fresh invading force of the microbes of that disease finds that defensive preparations have been made in advance. In the case of some diseases this acquired immunity is usually lifelong, as in that of small-pox; in others, of which influenza is a notable example, it is as a rule very transitory; and there are all gradations between the two. It is thought that this acquired immunity to some diseases may be transmitted to the offspring, for it is quite certain that there are many people who are from birth insusceptible to scarlet fever, no matter what may be the extent of their exposure to that disease.
The recognition of Nature’s elaboration of protective antitoxines has led to their artificial cultivation in the lower animals, and, thus produced, they have been used with brilliant results in the prevention and cure of at least one formidable disease, diphtheria. The immense reduction of the mortality from this disease that has followed the introduction of the treatment with the artificial antitoxine we owe to Behring, of Germany, and Roux, of France. Omitting unnecessary details, we may describe the process of obtaining diphtheria antitoxine as follows: A certain amount of diphtheritic poison (of the bacteriological sort, prepared by cultivating the diphtheria microbe) is injected into the circulation of a horse–sufficient to make the horse sick, but not enough to endanger his life. The horse’s system straightway begins to elaborate the protective antitoxine, and there results from this one injection a sufficient amount of it to save the horse, although far too little to make the serum of his blood potent enough for medicinal use. Hence, after the lapse of a suitable interval, he is again injected with diphtheritic poison, and for the second time his blood begins to generate the antitoxine. And the process is repeated again and again, the virulence of the poison being increased each time, until the horse’s blood is fairly reeking with antitoxine. Then blood is drawn freely from the horse, and it is allowed to separate into clot and serum, the latter alone being the part destined for use. This serum is tested on a small animal that has been inoculated with a deadly dose of the diphtheritic poison; if it saves the little creature from death, it is assumed to be potent enough for use on human beings, and, handled with all possible precautions against putrefaction or any contamination with pathogenic bacteria, it is furnished to physicians, its degree of potency being designated in “units.”
If in this brief article, which does not purport to be more than a sketch of the tremendous strides made by medicine in the Nineteenth Century, so much space has been given to the germ theory of disease, it is because the demonstration of the truth of that theory has been absolute, and has constituted the very marrow of almost all the medical progress of the century that has been the outcome of continuous thought and study as opposed to chance discovery.
Such results as the germ theory has now led to in the treatment of diphtheria it had already accomplished in the field of surgery as a consequence of that strict asepticism which, originating with Joseph Lister (now Lord Lister), and rapidly carried by him to a condition verging on technical completeness, was soon taken up by surgeons all over the world and brought wellnigh to perfection, so that the mortality of wounds of all sorts has been tremendously reduced, and many surgical operations are now practised frequently–indeed, whenever the occasion for them arises–that before the days of Listerism would have been looked upon as almost tantamount to the patient’s death-warrant. More particularly is this the case as to operations which involve opening into the abdomen, the chest, or the cranium. So little risk now attaches to such operations, properly performed, that the opening of the abdominal cavity for the mere purpose of ascertaining the condition of its contents–“exploratory laparotomy,” as it is called–is a matter of constant occurrence. Curiously enough, in some way not yet satisfactorily explained, that procedure in itself, without anything further being done, has in many instances resulted in decided amelioration of a morbid condition, if not in its cure. A striking example of this is seen in the benefit that often results in cases of one form of “consumption of the bowels,” namely, tuberculous disease of the membrane that lines the abdominal wall and invests the abdominal organs. This is not the only operation that does good mysteriously; that of cutting out a bit of the iris in a form of deep-seated eye disease, glaucoma, that tends toward complete blindness, is hardly more explicable; neither is an incision of the capsule of the kidney for certain forms of Bright’s disease, each of which stays the progress of the trouble in a goodly proportion of instances.
Another of the great divisions of the healing art, that of midwifery, has been enhanced quite as much as general surgery by the employment of Listerism. The process of childbirth, although a perfectly natural one, almost necessarily carries with it a certain amount of laceration, and, through the wound surfaces thus produced, absorption of poisonous material was formerly so frequent that puerperal fever figured prominently in mortality reports. It was Oliver Wendell Holmes–a graduate in medicine and a professor in the Harvard Medical School, though we are accustomed to think of him only as a delightful writer–who first declared that puerperal fever was the product of infection from without the body, and Semmelweis demonstrated the truth of the proposition. Holmes was a teacher of physiology, and his study of that branch of medical science was in itself enough to convince him of the doctrine which he inculcated.
Listerism must be credited, not only with having added immensely to the safety of the major operations of surgery, but also with having led to great improvement of their technics by reason of the greatly increased frequency with which it has come to be thought justifiable to practise them; what we do again and again we are apt in the end to do well, whereas that which we turn to only in despair and as rarely as possible, we do clumsily and imperfectly. Listerism has been unjustly alleged by a few to be unworthy of the appreciation in which it is held by the great majority of medical men of all countries; simple cleanliness, it has been urged, is quite as efficient as the full Listerian precautions. This is begging the question, for simple cleanliness, “chemical cleanliness,” is all that Listerism purports to accomplish. The use of antiseptics has been decried in the interest of asepticism, as if the whole purpose of antisepticism were not to secure asepsis. Lord Lister is entitled to the full credit of establishing the aseptic surgery of the present day, in spite of the facts that his doctrine followed rather than preceded his early improvements, that aseptic procedures have been brought nearer perfection elsewhere than in his own country, and that the whole system rests on foundations laid by Pasteur.
While it is quite true that to the Listerian theory and practice are almost wholly to be ascribed the favorable results of the major surgery of the present day, we must not forget the immeasurable benefits to the diseased, the injured, and the crippled that have arisen from patient efforts and occasional brilliant intuition that have had no connection with the germ theory of infection. Take the case of a broken leg, for example, an injury that formerly condemned the victim to weeks and weeks of confinement to bed, together with the suffering and danger almost inseparable from the old methods of the long straight splint and tight bandaging. At the present time he who has met with such a misfortune is commonly able to be about on crutches within a few days, and his broken bone mends while he is cultivating his appetite and indulging in pleasant intercourse with his fellow-men. This great change has been made possible by one device after another, invented by different men. Josiah Crosby introduced the use of sticking-plaster for extension, instead of the chafing bands previously employed; Gurdon Buck substituted elastic extension by means of a weight and pulley for the rude and arbitrary traction in vogue before; James L. Little devised the plaster-of-Paris splint, whereby broken bones were immobilized with hardly appreciable discomfort; and Henry B. Sands established the safety and practicability of applying the plaster-of-Paris splint almost immediately after the reduction (“setting”) of the fracture. In the meantime Nathan R. Smith and John T. Hodgen had demonstrated the advantages of suspending a fractured limb from above. All these men were Americans; surely our country has contributed powerfully to the well-being of the subjects of fracture. Other Americans, notably Lewis A. Sayre, have enabled sufferers with joint disease, including the dreaded hip disease, to run about and gain health and strength, instead of languishing in bed. Sayre, too, by his suspension treatment and the plaster-of-Paris jacket, set the hunchback on his feet at a stage in his disease in which before he had been forced to prolonged and painful recumbency.
Although men professing special skill in certain operations, and doubtless possessing it, flourished in old times, and left more or less of their impress on the surgery of the present day, for that matter, it was not until the second half of the Nineteenth Century that regional surgery (which is what specialism virtually amounts to) was systematically cultivated. Now there is hardly a portion of the body to which practitioners who make its ailments a specialty do not direct their searching methods of examination or on which they do not practise their ingenious devices in the way of treatment. Specialism has always been decried by a large section of the medical profession. On the other hand, it has been and is still overrated by the laity. The true estimate lies between the two. The specialists have advanced surgery immensely, but, with many honorable exceptions, they have laid too much stress on their several specialties, making too wide a range of ailments fall within them. As for the community at large, their shortcoming lies in the fact that most of them would seek for a specialist in mumps in case that painful but transitory infliction were to come upon them, and in their underrating of the family physician.
To change for a moment to a topic akin to the germ theory of disease, the reader may be reminded that the antitoxine treatment of infectious disease involves in almost every instance the use of some product contained in the serum (that is to say, the watery part of the blood). This leads to the subject of the use of natural and artificial serum in the treatment of disease. To quote again from the article entitled, “The Nineteenth Century in Medicine” (“New York Medical Journal,” Dec. 29,1900): “It has been observed that the normal serum of certain animals that are insusceptible to particular infectious diseases, if injected into the human blood current or even into the subcutaneous tissue, confers more or less of immunity against those diseases…. Artificial serum seems to have been first employed by Edmund R. Peaslee as a benign application to the peritonaeum in the operation of ovariotomy. His conception of its mode of action is not very clear, but he was a very successful ovariotomist, and we can only conjecture that he builded better than he knew, like many another man. A few years ago much was expected from transfusion of blood, but gradually the conviction has forced itself upon us that it is wellnigh useless, and indeed that, on the whole, it is worse than useless. It has virtually been abandoned…. But experiments in transfusion have not been fruitless; they have culminated in demonstrating the inestimable value of infusions of ‘normal,’ or ‘physiological,’ solutions of sodium chloride, and not only of infusions, but also of peritoneal irrigation with such solutions. Many a life has been saved by resorting to this measure, even in apparently desperate cases.”
Within about a decade of the close of the century, Robert Koch, whose discoveries and ingenious studies in bacteriology had brought him world-wide renown, announced that he had produced a derivative of the tubercle bacillus, which he termed tuberculin, that he thought might prove curative of tuberculous disease. It was to be injected beneath the skin. If the subject was really tuberculous, he would “react” by manifesting a certain degree of fever, and repeated injections would bring about elimination of the tuberculous deposits and thus effect a cure. The world was carried away with such an announcement coming from such a man, and it was thoroughly believed that at last “the great white plague,” consumption, was to be conquered. Tuberculin did, indeed, cure certain minor forms of tuberculous disease, such as the skin affection known as lupus, but it soon became evident that it was almost impotent in the treatment of pulmonary consumption. It has, however, served to enable the veterinarian to make out the existence of tuberculous disease in cattle at an early stage of its course, and it is probable that by the slaughter of cattle thus found to be tuberculous much infection of human beings has been prevented.
Tuberculin failed of its prime purpose, but it does seem to have marked the initiative of a campaign against consumption which has already proved of incalculable benefit, and bids fair to put that omnipresent disease toward the foot of the list of causes of death. We have made substantial advances in our knowledge of the disease, and we no longer regard it as incurable. We have learned that it is communicable from one person to another, but also that its communication can easily be prevented, so that there is no reason to shrink from association with tuberculous persons. We have learned, too, that consumption in one’s progenitors, immediate or remote, hardly makes it even probable that he himself is doomed to suffer with it; the only tuberculous heredity that we now recognize is that of defective ability to withstand the infection, and even this we regard as in most instances readily surmountable. We have learned, furthermore, that pulmonary tuberculous disease is by no means so fatal as it was formerly esteemed, for men whose business it is to make great numbers of post-mortem examinations, such as coroners’ physicians and hospital pathologists, assure us that in a very large percentage of cases of death from other causes they find indubitable signs of past tuberculous disease of the lungs which had ceased its activity–been, in fact, cured, either spontaneously or by medical intervention. Such intervention, it has been abundantly proved, is altogether likely to be successful if it is of the right sort and employed early. There is, to be sure, no cure-all. Powerful as the climatic treatment is, it must be supplemented by measures accurately adapted to the individual case, and failure to comprehend this fact still leads many a phthisical person to his grave. But information is rapidly being diffused, sanatoria for such of the tuberculous as can take advantage of them are multiplying, and those who are shut off from their aid are growing more and more cognizant of how they should live in order to give themselves the best chance of recovery and save their associates from infection. The era of consumption-cures–meaning drugs–is past; but the disease is cured in an ever-increasing proportion of instances, and that, too, by medical though not medicinal measures.
At almost every turn medicine has been powerfully assisted by the sciences which should rather be termed correlative than subsidiary. Notable among them is chemistry. The isolation of the active principles of medicinal plants–such as morphine, quinine, strychnine, and cocaine–has been a remarkable service rendered by chemistry to medicine. How should we be handicapped if we still had to fight malarial disease with the crude Peruvian bark instead of its chief alkaloid, quinine! And how impracticable if not impossible would it be to render the eye insensitive to pain with any extract of coca leaves, no matter how concentrated–a purpose that we accomplish almost instantly with cocaine! Of minor importance, perhaps, but not to be despised, is the resulting liberation from the old slavery to bulky and nauseous drugs. The isolation of active principles long antedated the synthetical preparations, but the latter came at last–the marvellous array of hypnotics, anodynes, and fever-quellers that are now at our command, largely coal-tar products. But it is not to pure chemistry alone that we are indebted for the elegant dosing of the present day; progressive pharmacy, with its tablets, its coated pills, and its capsules, has put to shame the old-time purveyor of galenicals. Right jauntily do we now take our “soda mint” in case of slight derangement of the stomach, happily oblivious of its vile prototype, the old rhubarb and soda mixture. Even castor oil has been stripped of its repulsiveness by the combinations which the soda water fountain affords.
It was but a step, we can now realize, from the employment of isolated vegetable principles to that of preparations of certain glandular organs of the animal economy, but the doctrine of “internal secretions” had to intervene, and its evolution took time; not till toward the close of the century did the venerable Brown-Séquard lead up to it. We have not yet come to “eye of newt and toe of frog,” but what we have incorporated into modern therapeutics in the way of animal products lends at least some theoretical justification to the ancient use of the dried organs of various animals. It is but a few years since the “ductless glands”–such organs, as, for example, the thyreoid gland (an organ situated in the front of the neck, a small affair in its normal state, but prominent and even pendulous when by its permanent enlargement it comes to constitute a goître)–were looked upon as puzzles, as structures destitute of any known function. Some observers even affirmed that they had no function, though the constancy of goître in cretins ought to have shown the fallacy of this allegation in the case of the thyreoid. We do not now need to be told that the thyreoid gland plays a very important part in the economy, for we know that its surgical removal gives rise to a special disease known as myxoedema, which, in addition to its physical manifestations, is characterized by impairment of the mental powers. Consequently, this ductless gland–a gland, that is to say, which has no obvious canal by which it throws off any product of its activity–must elaborate some material that is necessary to the health of the organism and is imparted to the blood. That material, whatever it may be, is termed an “internal secretion.” Some of the internal secretions have turned out to be of singular value medicinally. It is apparently not the ductless glands alone that furnish internal secretions; the glands that are provided with ducts and yield a definite and observable product secrete also a substance (perhaps more than one) which they give up to the blood.
Prominent among the therapeutic advances of the century is the direct reduction of the high temperature of sunstroke and certain fevers by the use of cold. Although foreshadowed by Currie early in the century by his use of cold affusion in the treatment of scarlet fever, it did not come into general use until the closing decades. It is employed principally in typhoid fever, on the theory that a condition of high fever is in itself a source of danger quite distinct from the other injurious effects of a febrile disease. On the other hand, the employment of high degrees of heat has of late been shown to be a potent agency in the treatment of certain forms of disease, notably in various affections classed as rheumatic. Applications of very hot air, provided it is thoroughly dry, are borne without serious discomfort, and their employment promises to be of greater service in the conditions in which it is resorted to than that of any other agent.
A revelation in the treatment of heart disease has been effected by the Bad Nauheim system of effervescent baths and resisted exercises. It is not only functional disorders of the heart that are relieved, but grave organic diseases also. Somewhat elaborate explanations of the way in which the treatment proves beneficial have been given, but they are not altogether satisfactory.
Thus far we have dealt chiefly with those developments of medicine that seem to have been the outgrowth of much thought and experiment, but there was one that can hardly be viewed as other than a happy discovery, yet it was one that was fraught with unspeakable mitigation of human suffering, and that wrought a boundless extension of the field of surgery. It was that of anaesthesia. The first to discover an efficient surgical anaesthetic was Crawford W. Long, of Georgia. It has been established that he performed several minor operations with the patient anaesthetized with sulphuric ether, but he did not proclaim his discovery, and so it was reserved for William T. G. Morton, of Boston (then a dentist, but subsequently a physician), to make the first public demonstration of the efficiency of ether as an anaesthetic, which he did in the operating theatre of the Massachusetts General Hospital, in Boston, in the year 1846. The news of Morton’s achievement spread broadcast, and it was at once realized that it was destined to revolutionize surgery. It certainly has done that, and in no less degree than was afterward accomplished by Listerism. Ether did not long remain the only anaesthetic known; Simpson, of Edinburgh, soon discovered that chloroform was possessed of even more decided anaesthetic properties. The inhalation of ether is disagreeable, and it is slow in producing the desired effect, whereas that of chloroform is not unpleasant, and it acts more rapidly. Consequently chloroform soon came to be generally preferred; but abundant experience has finally shown that ether is much the safer agent of the two, and improved methods of administration have almost entirely done away with the objections to its use, so that now it is looked upon as the preferable general anaesthetic. But general anaesthesia–meaning the suspension of sensibility in the whole organism, including unconsciousness–is not always necessary, and sometimes it is undesirable. We have now trustworthy local anaesthetics, the chief of which is cocaine, wherewith we are able to anaesthetize the part to be operated on without rendering the patient unconscious, and the co-operation that a conscious patient may be able to render is sometimes valuable. It was not alone in the direct saving of human suffering that anaesthetics proved a boon to the world; they have made possible an amount of experimental work on animals in the way of vivisection that humane investigators would otherwise have shrunk from, necessary as it has been and still is for the advancement of the healing art.
The operation of ovariotomy, first performed by Ephraim McDowell, of Kentucky, can hardly be classed with the happy accidents; but so little had been said about it or thought concerning it that when the news of it reached Europe “from the wilds of America” the editor of a ponderous English quarterly journal of medicine recorded his incredulity in the words “Credat Judoeus, non ego” An ovarian tumor inevitably proves fatal in the long run if it is not removed. In a certain percentage of cases it is malignant and will kill whether it is removed or not, but the general result of ovariotomy has been the saving of thousands of women from untimely death. Bell, of Edinburgh, had imagined the operation and had mentioned it in his lectures, but none the less to McDowell is due the credit of demonstrating its feasibility.
Medicine bore quite its full share in the mitigation of the horrors and hardships of war that marked the Nineteenth Century. Its work was shown in the great reduction of pestilential disease incident to camp life, in prompt aid to the wounded, in the establishment of salubrious field and general hospitals, and in improved methods of transportation of the sick and wounded. Certainly the soldier on the sick list never before had such a fair prospect of rejoining his comrades safe and sound as he has now.
In the care of the insane, too–care not only in the sense of humane treatment, but in the systematic employment of measures for their restoration to mental soundness–the century has been marked by notable progress. This has been chiefly in the direction of preventing insanity, and although mental disease is said to be on the increase, it may undoubtedly be said with entire truth that its growing prevalence is not in proportion to the heightened frequency of “the strenuous life.” We may confidently expect that a more pronounced mastery over diseases of the mind will come when physicians in general are taught psychiatry clinically, so that the beginnings of mental alienation may be intelligently met by the family practitioner.
The supreme achievement of the medicine of the Nineteenth Century undoubtedly has been the development of its preventive feature. When we recall the fact that but a few years ago an attack of infectious disease was interpreted as a visitation of Providence, by a perversity that even the triumphs of vaccination did not serve to do away with; when we contemplate the well-ordered and well-understood measures that are now resorted to in an ever-increasing number of communities (and resorted to not solely on the outbreak of an epidemic, but at all times), to purify the air we breathe, the food we eat, and the water we drink; and when we reflect upon the greatly reduced morbidity as well as mortality of most infectious diseases–we must realize the immense service that has been rendered by preventive medicine. No doubt we must all die some time, and the day is yet far remote when the only causes of death will be old age and injury; but a decided prolongation of the average lifetime, such as the life-insurance companies recognize, is an unquestionable gain to the human race.
A great blessing that has been brought about in great measure by medical men has been the establishment of the profession of nursing. The work of caring for the sick between the physician’s visits is no longer, at least in large communities and in cases of severe illness, left to over-sympathetic and uninstructed relatives or to outsiders who traded on mystery. An intelligent and intelligible record is now kept of all important happenings in the sick room, remedies are administered as they were ordered, needless alarm at something deemed by the patient to be of ill omen is quelled, and in case of real emergency, overlooked as it might otherwise have been, the physician is summoned to meet it. The advent of the trained nurse marked an era in medicine.
The literature of medicine has fully kept pace in volume with the progress of the art itself, and its quality has steadily improved. To this the great tomes of that gigantic work, the “Index-Catalogue of the Library of the Surgeon-General’s Office, United States Army,” bear solid testimony. It is a consolidated catalogue, by subjects and by authors’ names, of practically every medical book published throughout the world and of every article in the periodical literature of medicine. For its existence the world is indebted to Dr. John S. Billings, formerly a surgeon of high rank in the army and now the director of the New York Public Library, and for its continued existence to the United States Government, and it is to be hoped that Congress will never cease to provide adequately for its continued publication. Its completeness and its accuracy long ago led to its being prized everywhere.
There are some problems of which medicine has hardly yet entered upon the solution. Prominent among them is that of cancer. Little as we now know of the real nature of that disease, we know quite as much of it as we knew but a few years ago concerning other diseases equally destructive and far more prevalent, which, however, we have now practically mastered. Who can say that we shall not triumph over cancer while the Twentieth Century is still young? Our final triumph is indubitable.
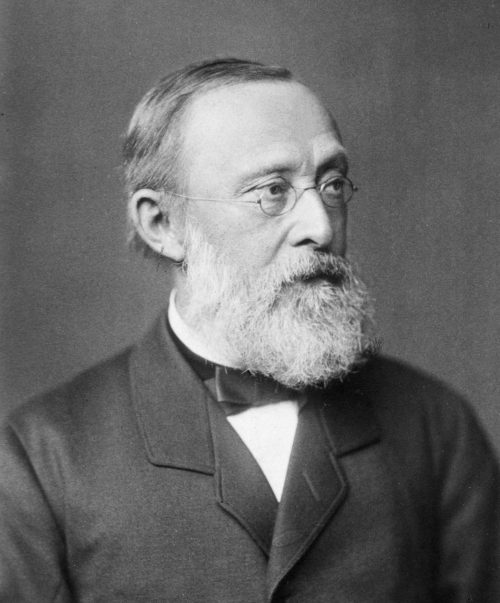
The strongest individuality in the medicine of the Nineteenth Century was without doubt that of Rudolf Ludwig Karl Virchow (commonly written by him simply Rudolf Virchow). Although he took no direct part in any of the striking advances in practice that appeal to the laity, yet he was recognized the world over, among all classes of educated and well-informed persons, as the one beacon light of Nineteenth-Century medicine whose glow had been the steadiest and the most enduring. This is because of the wide range of his learning in matters not pertaining closely to his profession. His professional brethren hold the same view, and this is because he so well controlled himself–checked himself at every turn by the severest application of system–that he continued for more than half a century an anchor to hold medical thought strictly down to fact. This was from no natural lack of volatility, for he was an Acht-und-vierziger (Forty-eighter). In 1846, as a prosector in the University of Berlin, Virchow entered with Reinhardt upon a series of pathological investigations which at once received wide attention. In conjunction with Reinhardt, he founded the Archiv für pathologische Anatomie und Physiologie und für klinische Medicin[6] (a periodical familiarly called “Virchow’s Archiv“), the publication of which was begun in the year 1847. Reinhardt died in 1852, leaving the editorship in the hands of Virchow alone, and he was still its editor up to the time of his death, on September 5, 1902.
In consequence of his having openly proclaimed himself a Democrat in 1848, Virchow was forced to retire from the University of Berlin in the following year. He was at once made a professor in the University of Würzburg, whence seven years later, in 1856, as the result of the strenuous interposition of various medical organizations, he was recalled to Berlin, where he was made a professor and director of the Pathological Institute. He was appointed medical privy councillor in 1874, having several years before that entered upon an active political career and been one of the founders of the Progressive party, which he ably represented in the Landtag and the Reichstag. In 1869 he took part in founding the German and the Berlin Anthropological Societies, of each of which he was several times president.
Virchow investigated the most diverse subjects, as his profound studies of Schliemann’s discoveries, as well as his other archaeological researches, show, and he was a rather prolific writer. The most important of his early works was Die Cellularpathologie, the first edition of which was published in 1858. Chance’s English translation appeared in 1860, and Picard’s French version came out in 1861. It is safe to say that no book of the century exerted a profounder influence on medical thought than Virchow’s exposition of the cellular pathology. His next notable publication was a collection of thirty lectures on Tumors (Die krankhaften Geschwülste,[7] Berlin, 1863-67). That he was not too absorbed in these lectures to bring his great powers to bear upon topics of the day is shown by the fact that before their publication was completed he brought out his work on Trichinae (Darstellung der Lehre von den Trichinen, 1864). Old age found him with industry and versatility unabated, for it was in 1892 that his Crania ethnica americana appeared, and after that time he wrote a vigorous protest against the new-fangled spelling of the German language which he accused the schoolmasters of trying to foist on the people. This was published in his Archiv. It may well be that his arguments have not been unavailing, since it is observable that several German publications that had adopted the new spelling have now dropped it.
It must not be supposed that it was by his literary work alone, founded though it was manifestly on his profound study, that Virchow impressed his personality upon medicine; it was in his lectures and in his laboratory teaching, too, that he made himself felt. In all civilized countries there are many devoted workers in medical science who caught their first real inspiration from Virchow.
The writer once saw Virchow–only once, but it was a sight never to be forgotten. It was at a banquet given as one of the festivities incident to the annual meeting of the British Medical Association in London in 1873. The company was not a large one, but it included such celebrities as Professor J. Burdon Sanderson, Sir William Jenner, Professor Chauveau, and Professor Marey. Virchow was conspicuously the man toward whom the eyes of all others were oftenest directed. Virchow met with the love as well as the admiration of his contemporaries, and both sentiments will descend to their successors, for his impress on the records of medicine is indelible, both as an instructor and as a friend of all real truth-seekers.
Authorities.
There is no full and connected account of the progress of medicine during the Nineteenth Century, but the reader may consult with profit the various medical biographies, also the following works: Silliman’s “A Century of Medicine and Chemistry;” Jenner’s “The Practical Medicine of To-day;” Buck’s “Reference Handbook of the Medical Sciences;” Eulenburg’s “Real-Encyclopädie der gesammten Heilkunde;” the “Annus Medicus,” published in the Lancet at the close of each year; and Tinker’s “America’s Contributions to Surgery” (Bulletin of the Johns Hopkins Hospital, Aug.-Sept., 1902).
[6] Archives of Pathological Anatomy and Physiology and of Clinical Medicine.
[7] Morbid Tumors.
John Lord – Beacon Lights of History, Volume XIV : The New Era